 [12]
[12] 

Spinal cord injury (SCI) is damage to the spinal cord, the bundle of nerves running from the base of the brain (brainstem) to the upper part of the lumbar spine. SCI disrupts communication between the brain and the rest of the body below the level of the injury, and depending on the severity resulting in the inability to move limbs, loss of sensation, bowel and bladder function. Depending on the underlying mechanism of injury, SCI can be divided into traumatic and non-traumatic causes. It can be further classified by the level of injury: tetraplegia involving all four limbs or paraplegia involving legs only; and the severity of injury: complete vs incomplete, with incomplete tetraplegia being most common.
Traumatic Spinal Cord Injury
Significant trauma to the vertebral column encasing the spinal cord can result in spinal cord injury. In a person with a vulnerable bony spine, for example someone with osteoporosis or ankylosing spondylitis, weakness in the supporting structure, such as with rheumatoid arthritis or Down's syndrome, or narrowing of the spinal canal due to spinal stenosis, a minor trauma or injury can result in spinal cord injury. The common underlying cause of injuries include motor vehicle accidents, followed by falls, violence such as gunshot wounds or assault, sports injuries, and industrial accidents. The A [1]merican Spinal Injury Association (ASIA) scoring system [2] is widely utilized by healthcare providers for further classification of SCI based on the injury level and severity.
Non-traumatic spinal cord injury
Spinal cord injury also can be secondary to multiple sclerosis (MS), inflammatory conditions, compression by bony spurs or herniated discs, and metastatic cancer, all disrupting spinal cord function. MS is a central nervous system (brain and spinal cord) disorder that damages the myelin sheath surrounding the nerve cells and fibers, and can presents with symptoms of spinal cord dysfunction, as well as disruption of vision, speech or cognitive function. A condition known as transverse myelitis is an inflammation across both sides of one level, or segment, of the spinal cord resulting in temporary or permanent symptoms that include paralysis and loss of sensation, bowel and bladder control. The segment of the spinal cord where the damage occurs determines the parts of the body affected, much like with a traumatic SCI.
SCI is a life changing event affecting a younger population (average age at injury: 42 years old) and it is a cause of major disability. Annual incidence of spinal cord injury is approximately 54 cases per million in the US, with approximately 17,000 new cases of SCI each year. The prevalence is estimated to be 282,000 persons alive with a SCI in 2016.1 Patients are initially admitted to acute care units of hospitals for stabilization for an average length of stay of 11 days followed by inpatient rehabilitation with an average 35 day length of stay.1,2 As cure is limited in most cases of SCI, patients require continuous outpatient care including intermittent physical, occupational and speech therapy, pain management, and prevention of complications directly or indirectly related to SCI including deep vein thrombosis, pressure ulcers, pneumonia and urinary tract infections.
Males account for approximately 80% of new SCI cases each year, with nearly 1 in 4 (22%) injuries occurring to non-Hispanic blacks since 2010, nearly twice the proportion of non-Hispanic blacks in the general population (12%).2
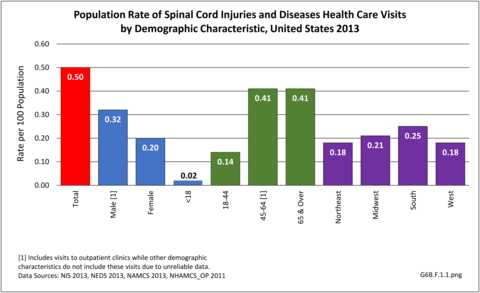
Analysis by demographic variables is limited by data size for outpatient clinic and physician’s office visits. However, as previously noted, males have a higher rate of SCI health care visits, and age is clearly a factor beginning in middle age around 45. Geographic region does not appear to be a factor. Race/ethnicity is unclear due to missing data cells. However, with a rate of 0.30 per 100 persons compared to 0.25 for all races, SCI health care visits appear to be greater among non-Hispanic whites than in other races/ethnicities. (Reference Table T6B.1.1 PDF [3] CSV; [4] Table 6B.1.2 PDF [5] CSV [6]; Table 6B.1.3 PDF [7] CSV; [8] and Table 6B.1.4 PDF [9] CSV [10])
In 2013, spinal cord injury or disease was diagnosed in 1.56 million health care visits, representing 1 person in every 200 in the US. However, it is likely more than one visit per person would reduce this ratio. Visits to outpatient clinics and physician’s offices generally do not meet standards of reliability, but for hospital discharges and emergency department visits with a diagnosis of spinal cord injuries and diseases, a diagnosis of ‘other paralytic syndromes’ account for 75% of visits. Nearly half (47%) of visits are to physician’s offices, while 1 in 5 (20%) involves hospitalization. (Reference Table 6B.1.5 PDF [13] CSV [14])
The mean age at the time of spinal cord injury increased from 29 years in the 1970s to 42 years in 2016.1 Non-traumatic spinal cord injuries are increasing, in part, due to the aging of the population and the concurrent age-related health conditions with a greater likelihood of minor events causing a SCI, like falls in an arthritic or stenotic spine. There is a possibility non-traumatic SCI will surpass the incidence of traumatic SCI in the future.2 The lifespan for SCI survivors has not changed since the 1980’s, and remains significantly shorter than for healthy counterparts. In 2016, for persons who survived the first 24-hours post injury, life expectancy for a 20-year old with the lowest level SCI is 52.6 years and for a 20-year old with a high tetraplegia 35.7 years. Comparable life expectancy for a 60-year old at time of injury is 17.9 years for a low level injury and 8.1 years for a high level tetraplegia, respectively.1 SCI survivors report more health problems, with significant impacts on physical function and quality of life posing greater challenges in aging SCI survivors.3
Mean hospital charges in 2013 for hospital stays with a diagnosis of spinal cord injury or disease were $80,700, with a mean stay of just over 8 days. Total hospital charges in 2013 were $25.7 million. Due to the severity of spinal cord injuries and diseases, this is only a small part of overall health care costs that usually last a lifetime. (Reference Table 6B.2.1 PDF [18] CSV [19]and Table 6B.2.2 PDF [20] CSV [21])
The average expense for the first year of injury in 2015 dollars, including health care costs and living expenses, ranges from $347,900 for the lowest level of injury to $1.1 million for a high tetraplegia. Average yearly expenses for each subsequent year of survival range from $42,300 to $185,100. These costs do not include indirect costs such as lost wages, fringe benefits, and productivity, which were estimated to be over $72,000 per year.1 In addition, there is significant economic and emotional burden to spouses and other family members.
Links:
[1] http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232636/
[2] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3232636/
[3] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.1.pdf
[4] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.1.csv
[5] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.2.pdf
[6] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.2.csv
[7] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.3.pdf
[8] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.3.csv
[9] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.4.pdf
[10] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.4.csv
[11] https://bmus.latticegroup.com/file/bmuse4g6bf11png
[12] https://bmus.latticegroup.com/docs/bmus_e4_G6B.F.1.1_0.png
[13] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.5.pdf
[14] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.5.csv
[15] https://bmus.latticegroup.com/file/bmuse4g6bf12png
[16] https://bmus.latticegroup.com/docs/bmus_e4_G6B.F.1.2_0.png
[17] https://www.nscisc.uab.edu/Public/Facts%202016.pdf
[18] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.1.pdf
[19] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.1.csv
[20] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.2.pdf
[21] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.2.csv