 [10]
[10] 

Motor neuron diseases (MNDs) are a group of rare disorders affecting motor neurons (nerve cells) that transmit signals from the brain to the muscles in the body. They present with muscle weakness and wasting, resulting in impaired walking, fine motor skills, limitations in activities of daily living, swallowing, speech, and eventually breathing. Motor neuron diseases can be classified into acquired (non-inherited) or inherited. There are no direct tests to identify MNDs, with diagnosis often the result of ruling out other conditions that early symptoms can mimic. In addition, there is no cure or standard treatment for MNDs. Generally, treatment consists of addressing symptoms, compensating for impairments, and providing palliative and supportive care. Some MNDs stabilize for long periods of time, while some rapidly progress to death in a few years.
Amyotrophic lateral sclerosis (ALS), often known as Lou Gehrig’s disease, is the most common type of motor neuron disease. It is usually rapidly progressive, has an unclear cause, and lacks a definite cure. According to the ALS registry, prevalence is 4 to 5 per 100,000 people, affecting more than 13,000 people1 Prevalence has been increasing over time due to better identification of cases. It is a fatal condition with short life expectancy after diagnosis.
The diagnosis of MND is made from the physician's interpretation of symptoms, while using selective diagnostic tests to confirm the diagnosis and rule out other mimicking conditions like spinal stenosis, cervical myelopathy or peripheral neuropathy. Diagnostic tests may include an EDx evaluation, lumbar puncture and MRIs of the spine and occasionally the brain. As there is currently no definitive cure for motor neuron disease, supportive care and prevention of unnecessary complications is the mainstay of management. Supportive care includes physical, occupational and speech therapy, respiratory care, nutritional and psychological support. Interdisciplinary care in a specialized center has been shown to provide superior care with slightly better survival in patients with ALS.1 Care is provided primarily at outpatient clinics, however, patients with debilitating symptoms require hospital admissions that are often lengthy and costly.2 Palliative care is required at the advanced stages of ALS.
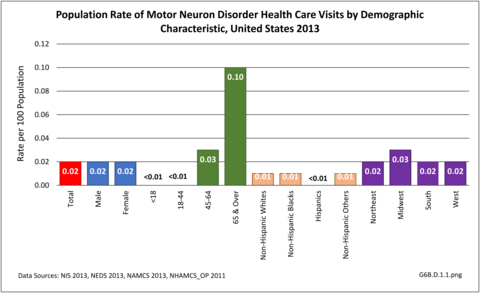
In 2013, 74,200 health care visits included a diagnosis of a motor neuron disorder. Because of the small number, the specific cause of the disorder could not be identified, and only hospital discharges and ED visits were of sufficient size to be included. An equal number of males and females were included, with the diagnosis more common among the aging population. Those 65 and over accounted for 60% of motor neuron disorder diagnoses, and ages 45 to 64 another 30%. Only hospital discharges were available by race/ethnicity, with non-Hispanic whites accounting for 74% of the diagnoses, compared to being 62% of the population. Geographic region in the US was not a major factor. (Reference Table T6B.1.1 PDF [1] CSV [2]; Table 6B.1.2 PDF [3] CSV [4]; Table 6B.1.3 PDF [5] CSV; [6] and Table 6B.1.4 PDF [7] CSV [8])
As previously noted, only discharges/visits from/to the hospital and emergency department had sufficient numbers to be analyzed; the two sites were evenly represented. (Reference Table 6B.1.5 PDF [11] CSV [12])
Incidence rates of ALS increase with age, peaking between 70 and 80 years. Amyotrophic lateral sclerosis is a fatal condition for most patients with mean life expectancy of about 3 years after diagnosis, although some patients live longer.
Poliomyelitis is a viral infection affecting the nervous system which causes motor neuron disease. Although it has been eradicated by vaccines developed in the 1950's, polio survivors can suffer from post-polio syndrome for several decades (mean of 36 years) with gradual weakness, fatigue and muscle wasting. A study published in 1994-1995 estimated there were about 1 million polio survivors in the U.S., with 443,000 reported having had paralytic polio. Considering 25 to 40 percent of polio survivors develop the post-polio syndrome, it is one of most prevalent motor neuron disease in the elderly population.1
It is difficult to estimate the economic costs related to motor neuron disorders due to their mixed presentation. However, due to the seriousness of these conditions, and the need for a broad range of treatments and supportive care, the burden of MNDs is significant compared to their prevalence. Nearly two-thirds (58%) of hospital discharges with a diagnosis of MND were discharged to additional care. Mean hospital charges for an average stay of 6.1 days were $55,000 (Reference Table 6B.2.1 PDF [15] CSV [16] and Table 6B.2.2 PDF [17] CSV [18])
Links:
[1] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.1.pdf
[2] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.1.csv
[3] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.2.pdf
[4] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.2.csv
[5] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.3.pdf
[6] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.3.csv
[7] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.4.pdf
[8] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.4.csv
[9] https://bmus.latticegroup.com/file/bmuse4g6bd11png
[10] https://bmus.latticegroup.com/docs/bmus_e4_G6B.D.1.1_0.png
[11] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.5.pdf
[12] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.5.csv
[13] https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2764727/
[14] https://www.ninds.nih.gov/Disorders/Patient-Caregiver-Education/Fact-Sheets/Post-Polio-Syndrome-Fact-Sheet
[15] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.1.pdf
[16] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.1.csv
[17] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.2.pdf
[18] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.2.csv