 [10]
[10] 

A focal neuropathy means only one or, at most, a few nerves are injured. Pain, numbness, and weakness are confined to a single limb or a small region of the trunk or head. Focal neuropathies are typically caused by compression or trauma. Carpal tunnel syndrome is an example of a focal neuropathy (as described below).
Mononeuropathy is a form of neuropathy that affects a single nerve or, more rarely, a nerve group (mononeuritis multiplex). There may or may not be pain, followed by loss of sensation, strength, and overall function, depending on the type. These types of neuropathies are typically due to injury, compression, aging, inflammatory disorders, or other systemic diseases. Examples of mononeuropathy include carpal tunnel syndrome, ulnar neuropathy, trigeminal neuralgia, radial neuropathy, peroneal neuropathy, radiculopathy, and occipital neuralgia.
Mononeuropathy can develop if there has been a prolonged period of swelling or pressure placed on a specific point in the body such as the hands, feet, or face. Symptoms of mononeuropathy include loss of feeling, tingling, burning, muscle weakness, and paralysis.
Mononeuropathy can develop if there has been a prolonged period of swelling or pressure placed on a specific point in the body such as the hands, feet or face. Symptoms of mononeuropathy include loss of feeling, tingling, burning, muscle weakness, and paralysis.
Carpal tunnel syndrome
Carpal tunnel syndrome is the most common mononeuropathy and is caused by entrapment of the median nerve in the carpal tunnel at the wrist. It is a slowly progressive condition causing tingling, numbness, and pain in the hand and fingers (possibly sparing the pinky finger), with weakness and wasting of muscle at the base of the thumb. Based on different studies, the incidence varies between 0.99 to 3.5 persons per 1,000 person-years.1,2 Higher incidence has been reported in women and working populations requiring repetitive wrist motions. Carpal tunnel syndrome is diagnosed based on clinical information (history and physical examination) and confirmed by electrodiagnostic tests (EDx) consisting of nerve conduction studies (NCS) and electromyography (EMG).
Ulnar neuropathy
Ulnar neuropathy is the second most common entrapment neuropathy and most commonly occurs at the elbow. It presents with weakness of the hand, along with tingling, numbness, and pain in the inner side of the hand and fingers (half of ring finger and pinky). It is often triggered from irritation of the “funny bone” where the nerve is exposed along the inner aspect of the elbow.
The brachial plexus is a network of nerves that originate in the neck and branch off to form most of the other nerves that control movement and sensation in the upper limbs, including the shoulder, arm, forearm, and hand. The radial, median, and ulnar nerves originate from the brachial plexus.
Brachial plexus injury (BPI) is an umbrella term for a variety of conditions that may impair function of the brachial plexus nerve network. Most pediatric and adult brachial plexus injuries are caused by birth or trauma respectively, such as high-speed vehicular or motorcycle accidents, blunt trauma, stab or gunshot wounds. It can also be the result of inflammatory processes, compression (e.g., caused by a growing tumor, thickened muscles, or the collar bone), or genetic mutation. Symptoms are pain, loss of sensation, muscle weakness, and varying degrees of paralysis.
Radiculopathy is a nerve root disorder that can cause numbness, tingling, pain, and weakness. It is typically caused by acute or chronic pressure on a nerve root as it exits the spinal canal. The most common cause is a herniated intervertebral disc in younger patients, and spinal stenosis, or narrowing of the spinal canal, in older patients. There are also several less common causes such as meningitis, tumors, diabetes, and infections.
Cervical radiculopathy typically causes pain radiating form the neck to the arm or shoulder blade region., often accompanied by tingling, numbness or weakness. The prevalence of cervical radiculopathy is 3.3 cases per 1000, with average age-adjusted incidence rate of .8 cases per 1000 persons. Lumbosacral radiculopathy typically presents as “sciatica”, pain radiating from the lower back into the buttock, thigh and/or leg. It is more common than cervical radiculopathy with a prevalence of 3% to 5% of the adult population, which is evenly distributed between men and women.3 Most radiculopathies related to disc herniation are self-limiting with symptoms resolving over the course of weeks to months.4
Carpal tunnel syndrome is the most common reason for electrodiagnostic test (EDx) referral.1
Conservative management includes activity modification, wrist braces, occupational therapy, and ultrasound guided steroid injections, . Carpal tunnel release to decompress the entrapped nerve is the primary surgical treatment and is commonly done if symptoms persist despite conservative management. The cost of treatment varies widely depending on the type of surgery, surgery setting, and amount of occupational therapy or lost work. Surgery is typically performed in an outpatient setting, and can be done open, with a camera or with a small incision under ultrasound. Potential complications include scarring, recurrent symptoms or nerve damage, although surgery is typically successful after appropriate diagnostic workup and conservative treatment.
Patients with radiating neck and back pain and neurologic deficits often require diagnostic studies such as MRIs and EDx to confirm the clinical impression, to investigate the underlying cause, and to determine severity. Although most radiculopathies respond to conservative management (oral pain medication, physical therapy, image guided epidural steroid injections), some patients require surgical treatment to decompress the nerve root.
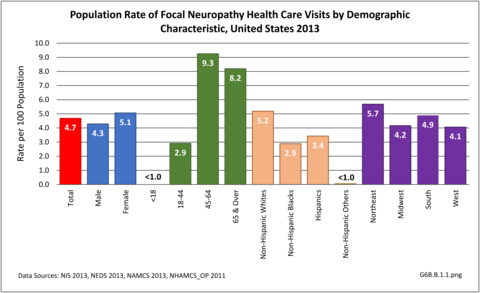
During 2013, there were more than 14.8 million healthcare visits made that included a diagnosis of focal neuropathy, representing nearly 1 in 20 persons in the US. Nearly all were adults over the age of 18, with most age 45 or over. Females were more likely to have a healthcare visit for focal neuropathy than males (55% of visits versus 45%), as were non-Hispanic whites. Non-Hispanic others accounted for less than 1% of focal neuropathy healthcare visits. Visits by geographic region were representative of the population. (Reference Table T6B.1.1 PDF [1] CSV [2]; Table 6B.1.2 PDF [3] CSV; [4] Table 6B.1.3 PDF [5] CSV [6]; and Table 6B.1.4 PDF [7] CSV [8])
Slightly more than 1.2 in 100 health care visits in 2013 had a focal neuropathy diagnosis. Most of these visits (84%) were to a physician’s office, where the rate of focal neuropathy diagnoses was nearly 1.4% of all visits. Only 3% of the total health care visits with a focal neuropathy diagnosis were hospital discharges, yet this accounted for 427,100 discharges. A diagnosis of root neuropathy was made in 3 out of 4 diagnoses. (Reference Table 6B.1.5 PDF [11] CSV [12]) (G6B.B.1.2)
As most entrapment neuropathies and radiculopathies increase with age, the burden of these conditions is increasing with the aging demographic profile of the US. The elderly were reported to have a higher prevalence of severe carpal tunnel syndrome.1 Due to age-related changes in the spine, the underlying etiologies of radiculopathy are different among various age groups. For example, radiculopathy from disc herniation is common in young adults, whereas spinal stenosis and spondylosis are more common in the elderly population.2
The burden of entrapment neuropathies and radiculopathy includes direct health care costs related to diagnosis, physical and occupational therapy, pain management, surgical intervention, plus indirect costs due to lost works days and productivity. Carpal tunnel syndrome is one of the most common worker’s compensation diagnoses. Radiculopathy from neck or low back conditions also significantly hampers mobility, activities of daily living, and quality of life.
Mean hospital charges for an average stay of 4.3 days in 2013 were $64,400, although this would not be actual cost paid due to variations in actual payments. Also, the hospital charges did not include professional fees and non-covered charges, such as lab tests. Adding to the cost for about one-third (36%) of discharges with a diagnosis of focal neuropathy discharged from a hospital in 2013 was “discharged to additional care”, either at a skilled nursing facility or with home health care. Mean emergency department charges were $3,200 with a focal neuropathy diagnosis, with 1 in 5 (19%) cases admitted to the hospital. (Reference Table 6B.2.1 PDF [15] CSV [16] and Table 6B.2.2 PDF [17] CSV [18])
Links:
[1] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.1.pdf
[2] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.1.csv
[3] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.2.pdf
[4] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.2.csv
[5] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.3.pdf
[6] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.3.csv
[7] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.4.pdf
[8] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.4.csv
[9] https://bmus.latticegroup.com/file/bmuse4g6bb11png
[10] https://bmus.latticegroup.com/docs/bmus_e4_G6B.B.1.1_0.png
[11] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.5.pdf
[12] https://bmus.latticegroup.com/docs/bmus_e4_T6B.1.5.csv
[13] https://bmus.latticegroup.com/file/bmuse4g6bb12png
[14] https://bmus.latticegroup.com/docs/bmus_e4_G6B.B.1.2_0.png
[15] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.1.pdf
[16] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.1.csv
[17] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.2.pdf
[18] https://bmus.latticegroup.com/docs/bmus_e4_T6B.2.2.csv